Megan Hodge’s first bout of intense pain arrived when she was in her mid-20s. Hodge and her husband were getting ready to visit family for Thanksgiving. Though Hodge had been dealing with a variety of chronic health issues, her workout had gone well that morning and she finally felt like she was getting a handle on her health.
Hodge began packing. As she reached into her closet to grab a sweater, her back gave out. The pain was excruciating, so intense that she felt light-headed and thought she might vomit.
As the years passed, Hodge had more frequent and more severe bouts of back pain. Any small movement could be a trigger — grabbing a towel from the linen closet, picking up a toy off the floor, sneezing. In 2021, Hodge experienced a particularly bad flare-up. None of the strategies she had previously used to help her manage seemed to be working. She was afraid to make any movement. She felt hopeless. “I just could not regain footing, metaphorically and physically,” she says. “I truly felt frozen in my chronic pain and chronic health journey.”
Hodge is far from alone. In the United States, chronic pain affects tens of millions of people — about 1 in 5 adults and nearly 1 in 3 people ages 65 and older. “The amount of suffering from arthritis and aging that I’ve seen in my pain clinic, it’s overwhelming to me as a pain doctor,” says Antje Barreveld, an anesthesiologist at Mass General Brigham’s Newton-Wellesley Hospital in Massachusetts. What’s more, the mainstay therapy for severe acute and chronic pain — prescription opioids — has helped fuel an epidemic that kills tens of thousands of people each year. “We have to have some better alternatives,” she says.
So researchers have doubled down in their quest to find new pain treatments that aren’t as addictive as opioids. “The pain field has really made very rapid and tremendous progress in the last decade,” says D.P. Mohapatra, a former pain scientist who now oversees research at the National Institute of Neurological Disorders and Stroke in Bethesda, Md.
The hope is that all the research will soon lead to new therapies. Vertex Pharmaceuticals is currently seeking regulatory approval for a new drug, suzetrigine, that looks promising in clinical trials. If approved, which could happen in early 2025, it would introduce the first entirely new class of pain therapies in decades. Though an initial approval would be for acute pain, there’s hope that the new drug could also curb chronic pain.
“Minor aches and pains, or even really painful acute pain, can largely be dealt with,” says Rajesh Khanna, a pharmacology researcher at the University of Florida in Gainesville. “But chronic pain? Unfortunately, there’s nothing.”
At the same time, there’s a growing recognition that treating chronic pain requires more than just pills. “We have a culture where people really turned to medications,” Barreveld says. “But there’s so much more to pain management than the pills that we prescribe.”
Pain researchers are also looking to non-pharmacological treatments, including devices that deliver pain-relieving stimulation and psychological strategies that help people manage their pain. The field is developing ways to boost existing therapies and working to identify the most effective combinations, as well as trying to figure out which patients might benefit most from which strategies.
“I think the future of pain care is going to be multicomponent therapy,” says Daniel Clauw, a pain researcher at the University of Michigan Medical School in Ann Arbor.
What is pain?
Pain is the warning system our body uses to try to protect us. It’s what makes you yank your hand away from a hot pan or hobble after twisting an ankle. Pain-sensing nerves in the periphery of the body called nociceptors identify potential threats — changes in temperature or pressure — and send electrical alerts zipping up to the brain. The brain processes these signals and then dials them up or down.
Clauw likes to compare the body’s pain system to an electric guitar. The peripheral nerves are the strings of the guitar, the brain is the amplifier. You can increase the volume by plucking the strings harder, or you can turn up the amplifier. If the brain decides the threat is real, it might enhance the pain.
“Then there’s the recovery process, where the body heals, and then you start to go back to normal,” says Tor Wager, a neuroscientist and psychologist at Dartmouth College. In most cases, the body desensitizes and recovers. The pain ebbs and disappears.
With chronic pain, though, the pain continues long after the initial trigger. In some cases, there is a clear physiological explanation and a clear solution. In other cases, neither the problem nor the solution is clear-cut.
“This pain is coming from the brain,” Clauw says. Fibromyalgia, a chronic condition that causes pain and fatigue, has become the poster child for this problem — what’s known as central sensitization — but, he adds, “most of the common chronic pain conditions are really now thought to be that mechanism.”
We have medicines to treat pain, of course. For mild to moderate pain, doctors often recommend nonsteroidal anti-inflammatory drugs, or NSAIDS, including aspirin or ibuprofen, for both acute and chronic pain. Antidepressants like duloxetine and anticonvulsants like gabapentin also seem to offer some relief for people with chronic pain. And doctors still turn to opioids.
But these medicines don’t work for everyone. And even when they do, they often provide only modest, short-term improvements. Even powerful opioids don’t eliminate chronic pain. A 2020 report by the U.S. Agency for Healthcare Research and Quality found little evidence for any long-term benefits of prescription opioid treatment. Clauw believes opioids may even make many types of chronic pain worse.
“We have this giant need for new treatments for pain,” says Stephen Waxman, a neurologist and pain researcher at the Yale School of Medicine.
New pain medications are hard to find
Developing new therapies to treat chronic pain has been tricky. In part that’s because a diagnosis doesn’t always shed light on the underlying mechanism. Is lower back pain caused by a compressed nerve, for example, or is it an amplifier problem? A treatment that addresses one may not work for the other.
What’s more, objective evidence that a medication is alleviating pain is hard to come by. There are no biomarkers, lab values or imaging results that can reliably measure pain. “You ask your patient to rate their pain from 0, no pain, to 10, the worst pain they can imagine. That’s a very noisy metric,” Waxman says. It depends on stress levels, sleep, mood, pain resilience and a litany of other factors. Plus, “the placebo response is somewhere between large and immense.”
Perhaps it’s not surprising then that the quest for new pain medicines has been beset by failures. Promising compound after promising compound has fizzled during development, including in late-stage trials. In 2021, Pfizer and Eli Lilly halted development of a promising antibody for arthritis and chronic back pain after regulators raised safety concerns.
Vertex’s new pain compound, suzetrigine, could be the first to deliver in a heated race to target specific sodium ion channels found on pain-sensing nerve cells (SN: 6/15/12). When these channels open, sodium enters the cell, decreasing the voltage between the cell’s interior and exterior. Eventually the voltage reaches a threshold, and the nerve sends an electrical impulse to the next nerve.
Scientists started chasing these channels seriously in the late 1990s, and the pace of research accelerated in the mid-2000s after researchers identified families who had a defect in a gene that codes for a particular sodium channel called Nav1.7. The defect cut pain off at the source.
Earlier this year, Vertex reported that suzetrigine, which blocks a related channel called Nav1.8, curbed pain better than a placebo in people who had just had tummy tuck surgery or bunion removal. But the compound wasn’t a slam dunk. In people who underwent bunion removal surgery, it didn’t work any better than the opioid hydrocodone combined with acetaminophen. And in tummy tuck patients, the opioid combination better alleviated pain.
Though pain medications that block sodium channels already exist — the anticonvulsant carbamazepine, for example — these compounds target a variety of sodium channels, not just those involved in pain. Blocking these channels causes side effects that limit the maximum dose. That’s why drugs like lidocaine and novocaine, which also block sodium channels, are injected locally.
“If you put them in the form of a pill, they block all of the sodium channels, including those in the heart and in the brain. So you get double vision, loss of balance, confusion, sleepiness,” Waxman says.
Though the effect of suzetrigine is “modest,” Waxman says, it’s a proof of principle: Targeting sodium channels specific to pain-sensing neurons works. And the hope is that the next generation of these compounds could be much better. In December, Vertex reported that the drug seems to alleviate pain in people with diabetic peripheral neuropathy, a kind of pain that stems from nerve damage typically in the hands and feet. This is an early step in extending suzetrigine’s potential use from acute to chronic pain.
Suzetrigine acts where pain begins, in the periphery. It can quiet the guitar strings, but it doesn’t directly address amplifier defects. Will fixing the peripheral component be enough to quell the pain? Waxman is hopeful, but it’s “an important intellectual question.”
New genetic discoveries may lead to more targets. Waxman has been studying people with a genetic condition called “man on fire” syndrome. Some people with this condition have overactive Nav1.7 channels that typically lead them to experience intense pain, but a subset of these individuals experience far milder pain than expected. He and his colleagues discovered that the individuals who experience milder pain harbor mutations in a gene that controls the activity of a family of potassium channels that act to stabilize neurons so that they don’t fire.
Waxman’s team is now working with a biotech company to develop a potential drug that would increase the activity of these channels in people who don’t have the mutations.
Pain-relief options beyond pills
Although many physicians are quick to prescribe pain medications, treating pain isn’t just about pills. In some cases, surgical procedures or injections can help relieve pain. Physical therapy can strengthen and stretch muscles and ligaments to curb pain. Neuromodulation therapies deliver electrical pulses directly to nerves to alleviate pain. Some, like spinal stimulation, are invasive. Others rely on electrodes placed on the skin.
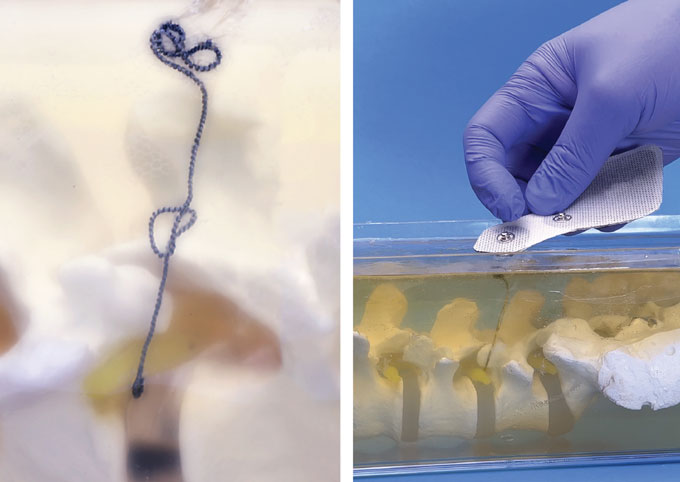
A team led by researchers at the University of Wisconsin–Madison has come up with a different, minimally invasive technique. The team developed an injectable electrode to create a pathway from the skin’s surface to nerves deep in the body’s tissue. This “injectrode,” currently being tested in people, enters the body as a flexible polymer-coated metal coil that can deliver electrical stimulation from a device outside the body to nerves deep in the tissues.
There is also a host of complementary and behavioral health therapies that can have a big impact on pain: acupuncture, meditation, yoga, massage, talk therapy — the list goes on and on. Many of these seem to work, at least in part, by addressing the amplifier problem. “The idea that your brain is actively creating pain, turning it up and down, facilitating spinal cord signaling of pain or dampening it, is really kind of a revelation over the past few decades,” says Wager, of Dartmouth. And it’s an idea that’s just beginning to percolate into mainstream medicine.
These therapies aren’t new. Cognitive behavioral therapy, for example, has been used to treat pain for decades. But researchers are turning to the latest discoveries in pain science to tweak these therapies to make them more accessible and more effective. Wager has developed a version of cognitive behavioral therapy called pain reprocessing therapy. It aims to help patients understand that chronic pain is often a construct of the brain and not necessarily a warning that needs to be heeded.
In a recent study of 151 people with chronic back pain, two-thirds of the people who received pain reprocessing therapy were pain free or nearly so, meaning their pain score was 0 or 1, at the end of the study, compared with 20 percent in the placebo group and 10 percent who received their standard care. And the effect lasted at least a year.
Talk therapy requires a serious time commitment. But Beth Darnall, a psychologist and pain scientist at Stanford University, is working on strategies that are more user-friendly. She is chief science adviser for AppliedVR, a company working to develop virtual reality tools to treat pain. The company’s program for back pain, called RelieVRx, teaches pain-relief strategies such as mindfulness, deep breathing and relaxation. The system also measures respiratory rate to provide participants with biofeedback.
“The world reflects back to them the changes that are occurring in their own body as they engage in a skill. And that’s pretty unique to be able to do that from home,” Darnall says.
In a recent trial, researchers assigned roughly 1,000 people with chronic lower back pain to receive RelieVRx or a sham virtual reality treatment for two months. Both groups experienced a reduction in pain, but the RelieVRx group reported a slightly larger drop, on average. (The sham treatment’s impact was attributed to the placebo effect.)
While the list of potential pain-relief options keeps growing, there is also an understanding that no single therapy or combination of therapies will work for everyone. “Pain is so complex and so diverse,” says Mohapatra, of the National Institute of Neurological Disorders and Stroke. “We cannot make pain therapy as a one size fit for all.”
Many patients have to find solutions through trial and error, which means it might be months or years before they find any relief. “Right now, we just fly blind,” Clauw says. What’s needed is a way to identify which therapies might work for which patients.
In 2019, the U.S. National Institutes of Health launched a study that aims to change that. The project, part of the NIH’s massive Helping to End Addiction Long-term — or HEAL — Initiative, will aim to find biomarkers to help predict which therapies will work for the most common and debilitating chronic pain condition: lower back pain. “It’s applying a precision medicine approach to low back pain for the first time,” Clauw says.
In one study, researchers will assign about 1,000 participants to one of four pain-relief strategies: an online education program; a kind of cognitive behavioral therapy known as acceptance and commitment therapy; physical therapy; or the pain medication duloxetine. Each participant will undergo an assessment that includes blood work, imaging of the spine and a physical exam. The hope is that these data can be used to create a model to predict which patient will benefit from which treatment — or more likely, treatments.
A multitreatment approach is what finally gave Hodge some relief. At the Shirley Ryan AbilityLab Pain Management Center in Chicago, she received comprehensive care that included physical therapists, occupational therapists, pain psychologists and physicians, all of whom collaborated and monitored her progress and well-being. “That’s not to say that I now live a life without any pain or without any flare-ups,” she says. “It’s not a cure-all.” But she does have a road map for how to deal with her pain, as well as the tools and mind-set to better navigate future flare-ups.
After Hodge graduated from the program, she wrote a letter to her care team about the impact of the skills she learned. “I am no longer constantly on edge, waiting for the other shoe to drop,” she wrote. “I finally feel safe in my body.”
#nextgen #pain #drug #shows #promise #chronic #sufferers #options
Image Source : www.sciencenews.org